|
Foot Ulcers
· An abscess (a pocket of pus) · A spreading infection of the skin and underlying fat (cellulitis) · A bone infection (osteomyelitis) · Gangrene (an area of dead, darkened body tissue caused by poor blood flow.) Individuals with chronic kidney diseases (CKD) are at high risk of foot ulceration and major lower extremity amputation. The risk status of any patient on dialysis should automatically be considered as being high, even in the absence of any active foot problems. A referral to a podiatrist for expert advice and treatment should occur if an active foot problem is discovered. |
Symptoms One of the first signs of a foot ulcer is drainage from the foot that might stain the socks. Other early symptoms include swelling, irritation, redness, and odours from the feet. The most visible sign of a serious foot ulcer is black tissue (called eschar) surrounding the ulcer. This is formed when there is an absence of healthy blood flow to the affected area of the foot. Partial or complete gangrene (tissue death due to infections) can also appear around the ulcer. In this case, odorous discharge, pain and numbness are common. Signs of foot ulcers are not always obvious. Some ulcers might not even show any symptoms until it is infected. Talk to your doctor or a podiatrist if you begin to see any skin discoloration, especially tissue that has turned black, or feel if you any pain around an area that appears callused or irritated. Your doctor may refer you to a podiatrist for treatment, or you can go directly to a podiatrist yourself. You do net need a referral to see a podiatrist. Treatment
The podiatrist will then apply a dressing. He or she may also prescribe specialized footwear to relieve pressure on the ulcerated area. This specialized footwear may be a cast, loosely fitting postoperative walking shoe or sandal that can be worn over a bandage. After the procedure, the foot must be examined frequently to debride the area. The dressing may also need to be changed every couple of days. Proper care of a foot ulcer can require multiple visits over weeks or even months. Medical attention of the foot is required till the ulcer has healed. Antibiotics may be prescribed to prevent the risk of infection. Once the ulcer has healed, your podiatrist may prescribe roomy, well-cushioned footwear. This footwear will prevent pressure on vulnerable areas of the feet and help prevent future ulcers. In certain situations, without leg surgery the ulcer may not heal properly. In cases where ulcers do not respond to more conservative therapy, surgery may be needed. People with poor circulation may need a procedure or surgery to open one or more blocked arteries in the legs. This may be done with angioplasty which involves threading a deflated balloon with a wire mesh cover (called a stent) into the blocked area. The balloon is then inflated -opening the artery. The stent stays in place to hold the artery open. For more significant blood flow problems, surgery is usually needed to re-route blood flow through the leg using a bypass artery. | Causes Foot ulcers are most commonly caused by:
Prevention Individuals with chronic kidney disease can take steps to help prevent foot ulcers. They should examine their feet routinely and follow good foot hygiene practices. The following may help prevent foot ulcers:
|




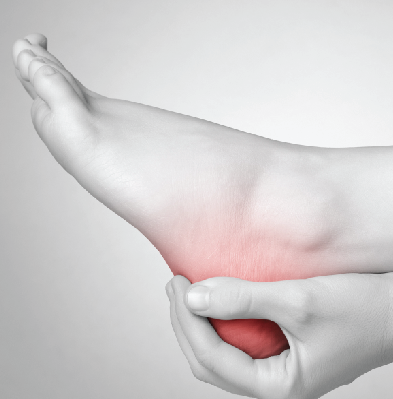 A foot ulcer is an open sore on the foot. Ulcers can be shallow, red craters that involve only the surface skin. However, they can also can be very deep. A deep foot ulcer may extend through all the layers of the skin. It may involve tendons, bones and other deep structures. If an infection occurs in an ulcer and is not treated right away, it can develop into:
A foot ulcer is an open sore on the foot. Ulcers can be shallow, red craters that involve only the surface skin. However, they can also can be very deep. A deep foot ulcer may extend through all the layers of the skin. It may involve tendons, bones and other deep structures. If an infection occurs in an ulcer and is not treated right away, it can develop into: If patients with proper circulation in foot foot, an ulcer may be treated with a procedure called debridement- trimming away diseased tissue and removing any nearby
If patients with proper circulation in foot foot, an ulcer may be treated with a procedure called debridement- trimming away diseased tissue and removing any nearby